Keratoconus is a corneal condition where the central or peripheral cornea becomes progressively thin and irregularly shaped.
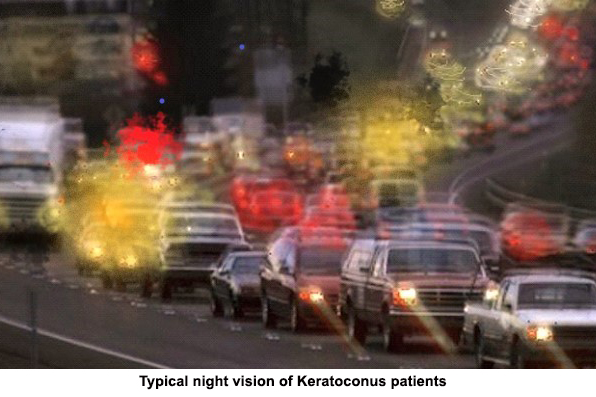 The surface of the cornea is where light begins its journey into the eye. The smoothness and shape of the cornea is vital to its function. Irregularly shaped surface scatters the light entering the eye and causes distorted vision.
The surface of the cornea is where light begins its journey into the eye. The smoothness and shape of the cornea is vital to its function. Irregularly shaped surface scatters the light entering the eye and causes distorted vision.
Although Keratoconus is variable in its progression for each individual, in some cases the dysfunction of vision can be devastating. Onset is often in early adolescence and it progresses into the mid-20’s and 30’s after which it stabilises. Majority of keratoconus are bilateral with each eye affected differently.
There is typically a history of frequent changes in vision that are not adequately corrected with eye glasses or soft contact lenses. Some patients experience intolerance to soft contact lens or unsatisfied vision correction with soft contact lenses. In advanced cases, patients’ vision is lost due to significant amount of glare, haloes and distortion.
Diagnosis can be made by slit-lamp examination and observation of inferior corneal protrusion. Unfortunately it is commonly misdiagnosed in mild cases. A computerised corneal topographer is useful in making an accurate diagnosis and assessment of its severity.
The goal of treatment is primarily to provide functional visual acuity. The options available are Specialty Lenses and Surgical Procedures
Specialty lens includes groups of lenses such as Corneal RGP Lens, hybrid lens and Scleral Lens.
They provide far superior vision in many keratoconus cases. The irregular cornea is normalized by the specialty lens with artificial solutions filled between the back of specialty lens and the cornea. Specialty lenses are customised to individual corneal surface irregularity based on computerised topography measurement.
Collagen Cross Linking (CXL)
Although there are no medicines that can prevent the keratoconus from progressing, Corneal Collagen Cross Linking (CXL) has been used in an attempt to make the cornea stronger in order to halt the keratoconus progression.
The procedure involves applying Riboflavin (Vitamin B2) to the eye and then using ultraviolet A (UVA) light for thirty minutes to activate Riboflavin in an effect to strengthen the bonds between cornea collagen. Our associated ophthalmologists can provide this surgical option for progressive keratoconus especially patients of the younger age group.
ICRS
Another surgical procedure is ICRS which is commonly known under their commercial names as Intacs or Kerarings or Ferrara rings. The procedure involves insertion of a plastic ring-shaped segment into the stroma of cornea.
However, ICRS does not slow down the procession of keratoconus. It aims to reduce the irregularity of the cornea to provide better vision quality without the need of other forms of correction. Although many cases have showed great vision improvement, specialty lenses are still required in most cases.
Transplant
Only a small percentage of patients ever require a corneal transplant.
Patients who loss vision function due to corneal scarring are candidates for corneal transplant. There are a few different types of transplant procedures depending on patients’ conditions. The procedure includes penetrating kertatoplasty (PK), Deep Anterior Lamellar Keratoplasty (DALK) , DSAK and DMEK. Our associated corneal specialists are available to assess your condition and discuss with you in details.
Although surgical procedures can stop the progression or partially improve visual function, in most cases, patients will still require specialty lenses to optimize their vision.
Copyright © Myopia Control Centre | Ortho-K Melbourne. All rights reserved